Total Knee Replacement
A knee replacement involves removing a thin layer of bone from the damaged surface of the femur (thigh bone), using special instruments which remove the correct thickness of bone. The removed bone is then replaced by a thin layer of metal, approximately the same thickness as the bone which was removed.
In a similar fashion the upper end of the tibia (shin bone) is removed and is replaced with a wafer of plastic. The back part of the knee cap (patella) may also be resurfaced with a piece of plastic.
In most cases, the three parts are attached to the bone by means of a bone cement. When this cement is first mixed it develops a dough-like consistency. This dough is pressed into the bone and the parts of the Prosthesis are pressed into the dough. The cement then hardens over 10 to 15 minutes into a plastic-like consistency.
After the knee has been replaced, the metal “cap” covering the end of the femur rubs against the plastic covering on the end of the tibia, preventing bone from rubbing on bone and giving relief from pain. The plastic is high density polyethylene a material which has a very low wear-rate and a very low frictional resistance when rubbing against the highly polished metal surface.
Total Hip Replacement
A hip replacement uses the combination of metal gliding on plastic, and cement to attach the artificial components to the bone. The arthritic head of the femur is removed and replaced with a metal ball which is attached to a metal stem. The stem is cemented into the hollow marrow space of the femur. The worn out hip socket is lined with a plastic cup, which is also cemented in place.
The painful parts of the arthritic hip are thereby completely replaced with metal and plastic surfaces. The plastic socket has a very low frictional resistance, and a very low wear rate against the metal ball.
With the development of the Cementless Hip Replacement the surface of the metal parts is porous, and looks like coral, hence bone can grow into the metal pores and lock the implant into place without the use of cement.
The Elbow
The elbow is a hinge joint made up of the humerus, ulna and radius.
The unique positioning and interaction of the bones in the joint allows for a small amount of rotation as well as hinge action. This rotation is easily noticed during activities such as hand-to-mouth eating motions.
One of the most common injuries to the elbow is called Lateral Epicondylitis, or Tennis Elbow.
Hand & Wrist

The hand is composed of numerous small bones called carpals, metacarpals and phalanges. The two bones of the lower arm — the radius and the ulna — meet at the hand to form the wrist.
The Shoulder
Shoulder Topics:
Shoulder Anatomy:
The shoulder provides more flexibilty than any other part of the body. The two main bones of the shoulder are the humerus and the scapula (shoulder blade).
The top portion of the scapula, the acromion, attaches to the clavicle, or collar bone. The end of the scapula, called the glenoid, holds the ball-like head of the humerus in place and acts as a flexible ball-and-socket joint.
Four short muscles originate on the scapula and pass around the shoulder where their tendons fuse together to form the rotator cuff.
Patient's Guide to Labral Tears
What is a Labral tear?
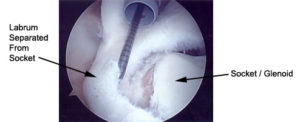
A Labral tear is a cause of shoulder pain. The labrum is a cartilage ring which surrounds the shoulder socket. The biceps tendon, which comes from the muscle on your arm, goes through the shoulder joint and attaches to the top of the labrum.
How does a Labral tear occur?
Many times, a Labral tear occurs from repetitive trauma in overhead throwers, such as baseball or volleyball. It can also occur from a traction injury to the arm, such as lifting a heavy object off the ground, or getting your arm jerked.
How do I know I have a Labral tear?
Many patients with a Labral tear have pain in the front of the shoulder or deep inside the joint. There also may be a feeling of catching or grinding in the joint. The examination in the office usually confirms the presence of a Labral tear.
Do I need x-rays, an MRI, or any other test?
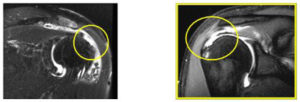
A set of x-rays is usually ordered to make sure there are no fractures in the shoulder. An MRI is helpful to confirm the tear of the labrum or biceps tendon, and evaluate other areas of the shoulder like the rotator cuff. My preference is to order something called an MRI Arthrogram. This is an enhanced MRI were they inject fluid into your shoulder, and if there is a tear the fluid will like into areas it does not belong. This is the best test for the confirmation of Labral tears.

Is there other damage to the shoulder in cases of Labral tears?
There can be other damage to the labrum seen with Labral tears, usually in the cases of shoulder instability. The biceps tendon itself can also be frayed or torn. Typically there is not a rotator cuff tear associated with this, but it is possible depending on how the injury occurred.
What are the treatment options for Labral tears?
The treatment primarily depends on your activity level and symptoms. Since Labral tears can often be difficult do diagnose, they are often first treated with physical therapy. The therapy is designed to restore range of motion and strength to the shoulder. Labral tears untreated do not heal because of the lack of blood supply in the area. In cases of persistent pain and disability, surgery is recommended.
How are Labral tears treated with surgery?
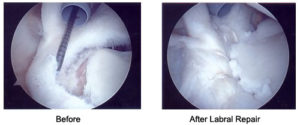
Labral tears are repaired arthroscopically. The arthroscope is a fiber optic instrument (narrower than a pen) which is put into the joint through small incisions. A camera is attached to the arthroscope and the image is viewed on a TV monitor. The arthroscope allows me to fully evaluate the entire shoulder joint, including the ligaments, the labrum, the biceps tendon, the rotator cuff, and the cartilage surface. Small instruments ranging from 3-5 millimeters in size are inserted through additional incisions so that I can feel the joint structures for any damage, diagnose the injury, and then repair, reconstruct, or remove the damaged tissue. With Labral tears, the damaged labrum is identified and then repaired back to the socket. This usually performed by using suture anchors to sew the labrum back in place. Occasionally, the biceps tendon is too damaged to repair. In this case, the tendon is cut and reattached in the upper arm (biceps tenodesis).
What are some of the possible complications?
While complications are not common, all surgery has associated risk. Possible complications include stiffness of the shoulder after surgery or recurrent pain. The use of arthroscopic techniques attempts to limit these complications. Other complications include an infection, bleeding, nerve damage, or problems with the anesthesia.
What do I need to do to prepare for surgery?
Our staff will help to set up the surgery through your insurance company and will instruct you on any paperwork that may be necessary. If you are over the age of 50, or have significant health conditions you may require an EKG and chest x-ray. You may also need to see your internist or family doctor to obtain a Letter of Medical Clearance. The day before the surgery, a member of the hospital or surgery center staff will contact you about what time to arrive for surgery. You may not eat or drink anything after midnight before your surgery.
How long will I be in the hospital?
Almost all patients are able to have surgery and go home the same day.
What happens the day of surgery?
The day before surgery you will be told what time to report to the hospital. You will be admitted and taken to a pre-operative holding area where you are prepared for surgery. You will be asked several times which extremity I am operating on, this question is asked many times on purpose.
After the operation, you will be taken to the recovery room to be monitored. Once the effects of anesthesia have worn off and your pain is under control, you will be given your post-operative instructions and a prescription for pain medication. Please be aware that the process of getting checked in, prepared for surgery, undergoing the operation, and recovering from the anesthesia takes the majority of the day. I would recommend that you and your family members bring some reading material to help make the process easier.
How should I care for my shoulder after surgery?
Prior to your discharge, you will be given specific instructions on how to care for your shoulder. In general you can expect the following:
Diet:
Resume your regular diet as soon as tolerated. It is best to start with clear liquids before advancing to solid food.
Medication:
You will be given a prescription for pain medication before you go home.

Sling:
You will have a sling, which you will use for the first 2 to 4 weeks. You can remove the sling for showering and performing your home exercise program.

Ice:
You should apply ice over the dressing for 30 minutes every 1 to 2 hours for several days. Sometimes we use a device called a Polar Care Cold Therapy Unit to help administer ice to your shoulder. Do not use heat the first week after surgery.
Suture Removal:
Sometimes absorbable sutures are used, they do not need to be removed. Occasionally, there are non-absorbable sutures, and they will be removed on your first post-operative visit.
Follow-up office visit:
You will be instructed on when to follow-up in the office. This is usually 2 weeks after surgery.
Exercise:
You will be instructed prior to your surgery on exercise to begin the day after your surgery.
Return to school or work:
You can return to school or work when your pain is under control, and you can perform the needed daily activities. If you need to use the arm to return, you may be out of work or school for a longer period of time.
What will rehabilitation involve?
The rehabilitation is based on several goals:
- Allowing the tissue to heal
- Regaining your range of motion
- Regaining strength
- Return to full duty at work, or return to sports
Sometimes a CPM (Continuous Passive Motion) Chair will be used post-operatively to help restore range of motion. You will attend PT 2-3 days per week.

When can I return to sports?
In general, you will be allowed to return to sports in 4 – 6 months after surgery. You must have good motion, strength, and control of your shoulder and arm. How quickly you return to sports depends on several factors, including:
- Your own rate of healing
- The damage found at surgery
- If you have any complications (like stiffness)
- How well you follow the post-operative instructions
- How hard you work in rehabilitation
When can I return to full duty at work?
You may return back to work in a matter of days, but on limited duty. In general I keep people on clerical duties for 3 months after the surgery, which means no lifting with your operated arm. This is to protect the repair. In the 3rd and 4th month I allow you to perform light duty meaning lifting no more than 10 pounds. People generally get back to performing full duty at work from 4 to 6 months.
What is the success rate?
The success rate for a Labral repair ranges from 85 to 95%. The goal is to achieve a shoulder with no pain for lifting, throwing, or overhead activity.
Call to make an appointment for one of the TOC Surgeons: (314) 336-2555
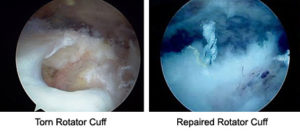
Patient's Guide to Rotator Cuff Injuries
What is the rotator cuff?
The rotator cuff is made up of four muscles and their tendons. The muscles attach at the shoulder blade (scapula) and extend out to form a cuff around the shoulder joint and insert at the upper portion of the arm (humerus). These four muscles are the supraspinatus, subscapularus, infraspinatus, and teres minor. These four muscles help to elevate and rotate the arm. In addition, these muscles help to stabilize the ball of the shoulder joint (humeral head) in the shallow socket of the shoulder blade (glenoid). The rotator cuff works especially hard to stabilize the shoulder when the arm is in the overhead position. This is why overhead activities can cause pain in someone with a rotator cuff injury.
What is a rotator cuff injury?
Most rotator cuff injuries are an inflammation of the tendon called tendonitis. The tendon gets overworked or sometimes gets pinched between the bones of the shoulder and becomes inflamed. This term is "impingement syndrome". In addition, there is a bursa which lies between the rotator cuff and the bone of the scapula (acromion). This bursa is a fluid filled sac that reduces the friction between the tendon and the acromion. Sometimes this subacromial bursa becomes inflamed along with the tendon, a condition called "bursitis".
Sometimes the tendonitis will progress to the point that the tendon becomes frayed or torn. Tears of the rotator cuff can be partial thickness tears only go part way through the tendon. Full thickness tears extend all the way through the tendon, and the tendon is detached from the bone. Once a rotator cuff tear has occurred they do not heal.
How is the rotator cuff injured?
Most commonly, the rotator cuff tendons wear and weaken with use until they eventually tear. In addition, in a tendon that already has some "wear and tear" a small amount of trauma, such as a pulling or lifting injury, can lead to a full thickness tear. Occasionally, there is a severe traumatic injury that also may cause the tear, such as an accident or fall. Rotator cuff tears occur most commonly in patients age 50 and older, and in people who play sports or perform a lot of overhead work.

How do I know my rotator cuff is injured?
Injuries to the rotator cuff most typically cause pain, especially with overhead activities. In addition, rotator cuff injuries or tears cause shoulder pain at night and lead to difficulty sleeping. Most patients that have a rotator cuff injury will complain of pain on the lateral or side of the shoulder. With large rotator cuff tears you may notice weakness in doing overhead activities. You may also have pain with activities of daily living, such as dressing, bathing, and reaching outward.
Do I need x-rays, a MRI, or any other test?
A set of x-rays is usually ordered to evaluate the bones around the shoulder. The bone above the rotator cuff, called the acromion, can be hooked, or have a bone spur, which leads to pinching and irritation of the rotator cuff. The x-rays are also used to evaluate for arthritis of the shoulder joint (glenohumeral joint), and acromio-clavicular joint (AC joint). A MRI Arthrogram may be ordered if a rotator cuff tear is suspected, or if the patient is not improving with conservative treatment.
Is there other damage to the shoulder when the rotator cuff is injured?
There is frequently other damage to the shoulder that can occur with rotator cuff injuries. The biceps tendon, which runs from the muscle in the front of the arm to the top of the shoulder joint, can become frayed or torn. You can also tear the labrum is a fibrous ring of tissue that surrounds the shoulder socket. In addition, the acromioclavicular joint, the joint on top of the shoulder, can become damaged or arthritic. Arthritis of the acromioclavicular joint commonly occurs along with rotator cuff injuries or tears.
What are the treatment options for rotator cuff injuries?
Many patients with a rotator cuff injury improve with conservative treatment. The treatment includes exercises, use of anti-inflammatory medications (NSAIDs), and possibly an injection of steroid (cortisone injection). The exercises may be a program you can do at home, or more commonly a formal physical therapy program. A cortisone injection is commonly used in patients that do not get better with therapy or in severe cases. Many patients get better with these treatments and do not need surgery. If patients do not get better with conservative therapy, or have an acute rotator cuff tear, surgery may be necessary.
How are rotator cuff injuries treated with surgery?
The surgery for rotator cuff injuries depends on the extent of the problem. Most rotator cuff tears can be repaired arthroscopically. The arthroscope is a fiber optic instrument (narrower than a pen) which is put into the joint through small incisions. A camera is attached to the arthroscope which allows me to fully evaluate the entire shoulder joint, including the ligaments, the rotator cuff, the labrum, and the cartilage surfaces. Small instruments ranging from 3-5 millimeters in size are inserted through additional incisions so that I can feel the joint structures for any damage, diagnose the injury, and then repair, reconstruct, or remove the damaged tissue.
For cases involving bad tendonitis or partial thickness rotator cuff injuries the entire procedure is done with the arthroscope. The under side of the acromion is shaved down (an acrmioplasty or decompression) which allows the rotator cuff to glide better, and not get pinched. If the rotator cuff is frayed, it is cleaned up (debrided).
For cases involving full thickness tears of the rotator cuff, the tear can sometimes be repaired completely arthroscopically. The bone is prepared for the tendon to be reattached, and then metal anchors (titanium suture anchors) are placed in the bone which contain sutures. These sutures are then weaved through the tendon, and the tendon is mobilized back to its bony attachment. These metal anchors are deep in the bone and do not need to be removed.
If the tear is large or longstanding, the surgery in rare cases needs to be performed with an open incision. This incision is placed in the area of the rotator cuff on the side of the shoulder, and the repair is performed with suture anchors and bone tunnels. This is called a "belts and suspenders" repair, which is the strongest repair that can be performed. This is called a "mini-open" rotator cuff repair.
What if I have pain or arthritis of my acromioclavicular (AC) joint?
Pain directly on top of the shoulder in the acromioclavicular (AC) joint can be treated with surgery. The surgery is to remove a small portion of the end of the clavicle bone, to eliminate rubbing between the bones. This then eliminates the pain. This procedure can be performed with the arthroscope or through a small 1 inch incision. There is no significant problem with arm strength when the end of the clavicle is removed.
What are some of the possible complications?
While complications are not common, all surgery has associated risk. Possible complications include stiffness of the shoulder after surgery or recurrent pain. Other complications include an infection, bleeding, nerve damage, or problems with the anesthesia.
What do I need to do to prepare for surgery?
Our staff will help to set up the surgery through your insurance company and will instruct you on any paperwork that may be necessary. If you are over the age of 50, or have significant health conditions you may require an EKG and chest x-ray. You may also need to see your internist or family doctor to obtain a Letter of Medical Clearance. The day before the surgery, a member of the hospital or surgery center staff will contact you about what time to arrive for surgery. You may not eat or drink anything after midnight before your surgery.
How long will I be in the hospital?
Almost all patients are able to have surgery and go home the same day. Occasionally, patients will be admitted for an overnight stay.
What happens the day of surgery?
The day before surgery you will be told what time to report to the hospital. You will be admitted and taken to a pre-operative holding area where you are prepared for surgery. You will be asked several times which extremity I am operating on, this question is asked many times on purpose.
After the operation, you will be taken to the recovery room to be monitored. Once the effects of anesthesia have worn off and your pain is under control, you will be given your post-operative instructions and a prescription for pain medication. Please be aware that the process of getting checked in, prepared for surgery, undergoing the operation, and recovering from the anesthesia takes the majority of the day. I would recommend that you and your family members bring some reading material to help make the process easier.
How should I care for my shoulder after surgery?
Prior to your discharge, you will be given specific instructions on how to care for your shoulder. In general you can expect the following:
Diet:
Resume your regular diet as soon as tolerated. It is best to start with clear liquids before advancing to solid food.
Medication:
You will be given a prescription for pain medication before you go home.

Sling:
You will have a sling, which you will use for the first 2 to 4 weeks. You can remove the sling for showering and performing your home exercise program.

Ice:
You should apply ice over the dressing for 30 minutes every 1 to 2 hours for several days. Sometimes we use a device called a Polar Care Cold Therapy Unit to help administer ice to your shoulder. Do not use heat the first week after surgery.
Suture Removal:
Sometimes absorbable sutures are used, they do not need to be removed. Occasionally, there are non-absorbable sutures, and they will be removed on your first post-operative visit.
Follow-up office visit:
You will be instructed on when to follow-up in the office. This is usually 2 weeks after surgery.
Exercise:
You will be instructed prior to your surgery on exercise to begin the day after your surgery.
Return to school or work:
You can return to school or work when your pain is under control, and you can perform the needed daily activities. If you need to use the arm to return, you may be out of work or school for a longer period of time.
What will rehabilitation involve?
The rehabilitation is based on several goals:
- Allowing the tissue to heal
- Regaining your range of motion
- Regaining strength
- Return to full duty at work, or return to sports.
When can I return to sports?
In general, you will be allowed to return to sports in 4 – 6 months after surgery. You must have good motion, strength, and control of your shoulder and arm. How quickly you return to sports depends on several factors, including:
- Your own rate of healing
- The damage found at surgery
- If you have any complications (like stiffness)
- How well you follow the post-operative instructions
- How hard you work in rehabilitation
When can I return to full duty at work?
In general I keep people on clerical duties for 3 months after the surgery, which means no lifting with your operated arm. This is to protect the repair. In the 3rd and 4th month I allow you to perform light duty meaning lifting no more than 10 pounds. People generally get back to performing full duty at work from 4 to 6 months.
What is the success rate?
The success rate for a rotator cuff repair ranges from 85 to 95% for attaining pain relief. If weakness is a significant problem, the results for regaining strength can be more variable.
To schedule an appointment with one of our shoulder specialist please call: (314) 336-2555.
The Spine

The spinal column is one of the body's main supports. The spine itself is divided into three sections: the cervical, the thoracic, and the lumbar spine. These sections are made up of interlocking vertebrae, which allow the backbone some flexibity.
Lumbar vertebrae are the strongest, they must support the weight of the upper body. Between the vertebrae are discs made up of cartilage that act as shock absorbers to prevent damage from sudden jolts.
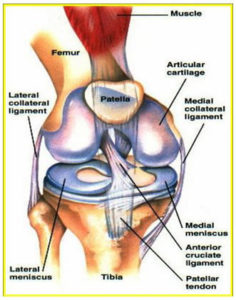
The Knee
Knee Topics:
Knee Anatomy:
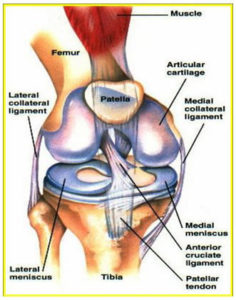
The knee is the body's largest joint. It consists of the femur and the tibia, which meet to form a hinge joint.
The joint is protected by the patella (kneecap), and cushioned by articular cartilage that covers the ends of these bones.
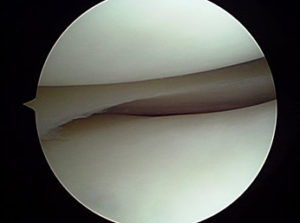
Patient's Guide to Knee Arthroscopy
What is arthroscopy?
The arthroscope is a fiber optic instrument (narrower than a pen) which is put into the knee joint through two small incisions. A camera is attached to the arthroscope and the image is viewed on a TV monitor. The arthroscope allows me to fully evaluate the entire knee joint, including the knee (patella), the cartilage surfaces, the meniscus, the ligaments (ACL & PCL), and the joint lining. Small instruments ranging from 3-5 millimeters in size are inserted through the incisions so that I can feel the joint structures for any damage, diagnose the injury, and then repair, reconstruct, or remove the damaged tissue. Before the development of arthroscopy, large incisions had to be made over the knee joint to treat or diagnose injuries. Today's arthroscopic techniques allow more complete evaluations of the knee joint while accelerating the rehabilitation process.
What kinds of procedures can be performed with the arthroscope?
Arthroscopy allows the surgeon to view the inside of the knee joint and perform a variety of surgeries. These surgeries include:
- Complete evaluation of the joint (diagnostic arthroscopy)
- Removal of damaged or torn cartilage (partial meniscectomy)
- Repair of torn cartilage (meniscus repair)
- Smoothing of damage to the cartilage surface in arthritis (chondroplasty)
- Realignment of patella in patellar mal-tracking (lateral release)
- Removal of joint lining (synovectomy)
- Replacement of articular cartilage (cartilage transplant)
What are some of the possible complications of surgery?
While complications are not common, all surgery has associated risks. Possible complications include stiffness of the knee after surgery or continued pain. The use of arthroscopic techniques attempts to limit these complications. Other complications include infection, bleeding, nerve damage, blood clots, or problems with the anesthesia. If a meniscus repair is performed, it is possible that the torn area will not heal. This would require a second surgery to remove the torn meniscus. Even though this is possible, it is better to attempt to repair a meniscus that may heal, in order to preserve the normal meniscus function.
What kind of anesthesia is used?
Knee arthroscopy can be performed with general anesthesia (going to sleep), or regional anesthesia (spinal or epidural block). The type of anesthesia will depend on your choice. The anesthesiologist will discuss your options the morning of surgery.
What do I need to do to prepare for surgery?
Our staff will help to set up the surgery through your insurance company and will instruct you on any paperwork that may be necessary. If you are over the age of 50, or have significant health conditions you may require an EKG and chest x-ray. You may also need to see your internist or family doctor to obtain a Letter of Medical Clearance. The day before the surgery, a member of the hospital or surgery center staff will contact you about what time to arrive for surgery. You may not eat or drink anything after midnight before your surgery.
How long will I be in the hospital?
Knee arthroscopy is an outpatient procedure you will go home the same day.
What happens the day of surgery?
The day before surgery you will be told what time to report to the hospital or surgery center. You will be admitted and taken to a pre-operative holding area where you are prepared for surgery. You will be asked several times which extremity I am operating on. Please note that you are asked this question many times on purpose.
After the operation you will be taken to the recovery room to be monitored. Once the effects on anesthesia have worn off and your pain is under good control, you will be given your post-operative instructions and prescription for pain medication and released.
Please be aware that the process of getting checked in, prepared for surgery, undergoing the operation, and recovering from anesthesia takes the majority of the day. I would recommend that you and your family members bring along some reading material to make the process easier for all.
How should I care for my knee after surgery?
Prior to your discharge, you will be given specific instructions on how to care for your knee. In general you can expect the following:
Medication:
You will be given a prescription for pain medication.
Showering:
You may shower, but you should keep the dressing dry. After your dressing is removed, 2-3 days post-op you may get your knee wet. You cannot take a bath until the wounds are completely sealed, usually 2-3 weeks after surgery.
Crutches:
You will be instructed how to use crutches before the surgery. You should bring a set of crutches with you to the surgery. How long you use crutches will depend on the type of surgery performed. Crutches are commonly only required for a couple of days, unless you had a meniscus repair, in that case I will let you know how long you should stay on your crutches to protect the repair.
Brace:
If a meniscus repair is performed, you will receive a brace to restrict the motion of your knee. This is to protect the repair for the first 4-6 weeks, to allow the area to heal.
Diet:
Resume your regular diet as soon as tolerated. It is best to start with clear liquids before advancing to solid food.
Ice:
You should apply ice over the dressing for 20 -30 minutes every hour for several days. Do not use heat for the first 48-72 hours.
Suture removal:
Some stitches are absorbable and do not need to be removed. However, if there are stitches they will be removed on your first post-op visit.
Return to work or school:
You can return to school or work anywhere from 2 days to 2 weeks. If you job involves more extended walking or heavy activity, you may be out of work or school for a longer period of time.
What will rehabilitation involve?
The rehabilitation is based on several goals:
- Allowing the tissue to heal
- Regaining motion
- Regaining strength
- Return to sports or work activity
After partial meniscectomy, the rehabilitation generally occurs very rapidly. Most patients can return to strenuous work in four to six weeks. However, you complete recovery may take 2-3 months to get all your strength back. Following meniscus repair, you will be restricted from performing certain activities. The specific rehabilitation protocol will be reviewed with you after surgery.
When can I return to sports or full duty at work?
Your return to your desired activity level will depend on the extent of damage and the procedure performed on your knee. In general, you will be allowed to return to sports in 4-8 weeks after surgery. You must have good motion, strength, and control of your knee. How quickly you return depends on several factors, including:
- Your own rate of healing
- The damage found at surgery
- If you have any complications
- How well you follow the post-operative instructions
- How hard you work in rehabilitation
Call to make an appointment for one of the TOC Surgeons: (314) 336-2555
Patient's Guide to Meniscus Injuries
What is the meniscus?
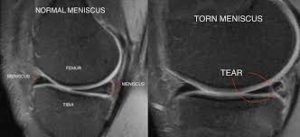
The meniscus is a wedge shaped cartilage ring found on both the inside and outside of the knee between the femur (thigh bone) and tibia (shin bone). The menisci act as shock absorbers in the knee, and provide stability to the joint.
How is the meniscus injured?
The meniscus is usually injured by twisting on a planted foot or squatting down and forcefully bending the knee. Occasionally, the tear occurs with very little stress on the knee. The tear can also be degenerative, meaning that the tear occurs because the tissue is worn out over time due to arthritis in the knee.
How do I know my meniscus is torn?
Most tears of the meniscus lead to knee pain in the area of the tear, on the inside or outside of the knee. Swelling of the knee may also occur, as well as pain that can radiate down the leg. Occasionally, locking and catching of the knee can occur, when the meniscus gets wedged in between the bones of the knee. Pain and instability caused by the meniscus tear can also cause the knee to buckle or "give way". Twisting activities usually worsen the symptoms.
Do I need x-rays, a MRI, or any other tests?
A set of x-rays may be ordered to evaluate the knee for arthritis or a fracture of the bones. Many times the diagnosis of a meniscus tear can be made through the examination in the office. However, in most cases a MRI can be helpful to confirm the tear and rule out any other injuries to the knee.
Is there usually any other damage to the knee when the meniscus is torn?
Ligaments in the knee can be injured at the same time as the meniscus, depending on how your knee was injured. In addition, there can be an injury to the joint surface (articular cartilage) at the time of injury. If surgery is required, damage to the joint surface will be evaluated and treated at the time of your arthroscopy.
What treatment options do I have?
Some people with meniscus tears will respond to conservative treatment, including rest, medications, and physical therapy. Meniscus tears do not heal, and over a period of time your knee joint will grind out the tear. In some cases, cortisone injection can also be helpful to resolve the pain and swelling. Whether or not you are a good candidate for conservative treatment will depend on the type of tear, age of the tear, and your desired activity level. Most people that have a meniscus tear go on to have a knee arthroscopy to help to resolve their symptoms.
How is the surgery performed?
Meniscal surgery is performed by arthroscopy. The arthroscope is a fiber optic instrument (narrower than a pen) which is put into the knee joint through two small incisions. A camera is attached to the arthroscope and the image is viewed on a TV monitor. The arthroscope allows me to fully evaluate the entire knee joint, including the kneecap (patella), the cartilage surfaces, the meniscus, the ligaments (ACL & PCL), and the joint lining. Small instruments ranging from 3-5 millimeters in size are inserted through the two portals so that I can feel the joint structures for any damage, diagnose the injury, and then repair, reconstruct, or remove the damaged tissue.
Before the development of arthroscopy, large incisions had to be made over the knee joint to remove the entire meniscus. Today's arthroscopic techniques allow more complete evaluations of the knee joint while allowing me to only remove the damaged portion of the meniscus, or to repair the meniscus if possible.
What is the difference between partial meniscectomy and meniscal repair?
Depending on the type of tear, the piece of meniscus that is torn may be removed from the knee (partial meniscectomy) or repaired (meniscus repair). Whether or not a tear is repaired depends on the likelihood of the tear healing. If a tear occurs in the outer one-third of the meniscus (peripheral tear), there is usually adequate blood supply for the tear to heal if fixed. However, tears in the inner two-thirds (where most tears occur) have no blood supply, and will not heal with repair. Therefore, the torn piece needs to be removed. Every effort is made to try and repair a tear that may heal. If the tear is repaired the overall recovery time is increased because I have to protect that repair.
Don't I need my meniscus?
It is always best to have your own normal meniscus. For this reason, every attempt is made to repair a meniscus tear that may heal. However, for tears that are torn beyond repair, it is best to remove the torn piece. The piece that is torn does not function like a normal meniscus, so removing that piece does not decrease the amount of functioning meniscus. Leaving a torn piece may irritate the knee joint and cause the tear to get larger. Only the portion of the meniscus that is torn or diseased is removed.
What are some of the possible complications of surgery?
While complications are not common, all surgery has associated risks. Possible complications include stiffness of the knee after surgery or continued pain. The use of arthroscopic techniques attempts to limit these complications. Other complications include infection, bleeding, nerve damage, blood clots, or problems with the anesthesia. If a meniscus repair is performed, it is possible that the torn area will not heal. This would require a second surgery to remove the torn meniscus. Even though this is possible, it is better to attempt to repair a meniscus that may heal, in order to preserve the normal meniscus function.
What kind of anesthesia is used?
Knee arthroscopy can be performed with general anesthesia (going to sleep), or regional anesthesia (spinal or epidural block). The type of anesthesia will depend on your choice. The anesthesiologist will discuss your options the morning of surgery.
What do I need to do to prepare for surgery?
Our staff will help to set up the surgery through your insurance company and will instruct you on any paperwork that may be necessary. If you are over the age of 50, or have significant health conditions you may require an EKG and chest x-ray. You may also need to see your internist or family doctor to obtain a Letter of Medical Clearance. The day before the surgery, a member of the hospital or surgery center staff will contact you about what time to arrive for surgery. You may not eat or drink anything after midnight before your surgery.
How long will I be in the hospital?
Knee arthroscopy is an outpatient procedure you will go home the same day.
What happens the day of surgery?
The day before surgery you will be told what time to report to the hospital or surgery center. You will be admitted and taken to a pre-operative holding area where you are prepared for surgery. You will be asked several times which extremity I am operating on. Please note that you are asked this question many times on purpose.
After the operation you will be taken to the recovery room to be monitored. Once the effects on anesthesia have worn off and your pain is under good control, you will be given your post-operative instructions and prescription for pain medication and released.
Please be aware that the process of getting checked in, prepared for surgery, undergoing the operation, and recovering from anesthesia takes the majority of the day. I would recommend that you and your family members bring along some reading material to make the process easier for all.
How should I care for my knee after surgery?
Prior to your discharge, you will be given specific instructions on how to care for your knee. In general you can expect the following:
Medication:
You will be given a prescription for pain medication.
Showering:
You may shower, but you should keep the dressing dry. After your dressing is removed, 2-3 days post-op you may get your knee wet. You cannot take a bath until the wounds are completely sealed, usually 2-3 weeks after surgery.
Crutches:
You will be instructed how to use crutches before the surgery. You should bring a set of crutches with you to the surgery. How long you use crutches will depend on the type of surgery performed. Crutches are commonly only required for a couple of days, unless you had a meniscus repair, in that case I will let you know how long you should stay on your crutches to protect the repair.
Brace:
If a meniscus repair is performed, you will receive a brace to restrict the motion of your knee. This is to protect the repair for the first 4-6 weeks, to allow the area to heal.
Diet:
Resume your regular diet as soon as tolerated. It is best to start with clear liquids before advancing to solid food.
Ice:
You should apply ice over the dressing for 20 -30 minutes every hour for several days. Do not use heat for the first 48-72 hours.
Suture Removal:
Some stitches are absorbable so they do not need to be removed.. However, if there are stitches they will be removed on your first post-op visit.
Exercise:
You will be instructed on exercises you can begin immediately after the surgery.
Return to work or school:
You can return to school or work anywhere from 2 days to 2 weeks. If you job involves more extended walking or heavy activity, you may be out of work or school for a longer period of time.
What will rehabilitation involve?
The rehabilitation is based on several goals:
- Allowing the tissue to heal
- Regaining motion
- Regaining strength
- Return to sports or work activity
After partial meniscectomy, the rehabilitation generally occurs very rapidly. Most patients can return to strenuous work in four to six weeks. However, you complete recovery may take 2-3 months to get all your strength back. Following meniscus repair, you will be restricted from performing certain activities. The specific rehabilitation protocol will be reviewed with you after surgery.
When can I return to sports or full duty at work?
Your return to your desired activity level will depend on the extent of damage and the procedure performed on your knee. In general, you will be allowed to return to sports in 4-8 weeks after surgery. You must have good motion, strength, and control of your knee. How quickly you return depends on several factors, including:
- Your own rate of healing
- The damage found at surgery
- If you have any complications
- How well you follow the post-operative instructions
- How hard you work in rehabilitation
Call to make an appointment for one of the TOC Surgeons: (314) 336-2555
Patient's Guide to ACL Injuries
What is the Anterior Cruciate Ligament (ACL)?
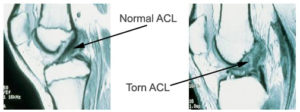
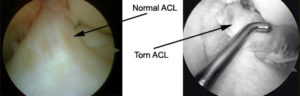
The anterior cruciate ligament (ACL) is one of the main ligaments in the center of the knee. It runs from the front of the tibia (shinbone) to the back of the femur (thighbone). It assists in proper movement of the knee joint, and prevents the tibia form slipping forward on the femur. Abnormal translation can create and unstable knee that "gives way" during activity.
How is the ACL injured?
The ACL is most commonly injured during a twisting or pivoting episode of the knee when the foot is planted on the ground. This can occur during such sports as football, soccer, basketball, or skiing. It can also be injured during a direct blow to the knee, or with hyperflexion or hyperextension of the knee.
How do I know my ACL is injured?
Usually a tear of the ACL results in sudden pain and giving way of the knee. Many patients report having felt or heard a "pop" when they injure their knee. In addition, the knee commonly swells within the first 1 to 3 hours after the injury. If the injury to the ACL is more chronic in nature, the injury most commonly leads to shifting or giving way of the knee with activity.
The examination in the office usually can almost always determine when there is significant ACL injury, by testing the ability of the ligament to prevent the tibia from moving forward on the femur. If the injury just recently occurred, it can be difficult to tell if the ligament is injured because the patient does not like the knee to be moved around during the examination.
Do I need x-rays, MRI, or any other test?
A set of x-rays is usually ordered to evaluate the bones around the knee. The x-rays are primarily used to evaluate for fractures or arthritis about the knee. A MRI may be ordered to look for damage to the ACL and rule out any other injuries to the knee such as a meniscus tear or bone bruise. Other ligament or cartilage injuries can occur in combination with injuries to the ACL, which can be seen on the MRI. A KT-1000 Knee Ligament Arthometer is another test commonly performed in the office to evaluate how unstable the knee may be.
Is there other damage to the knee when the ACL is injured?
Other ligaments in the knee can be injured at the same time as the ACL. The most common ligament to also be injured is the medial collateral ligament or MCL. This ligament is on the inside of the knee, and prevents the legs from moving inward.
In many cases there is a meniscus tear that occurs at the time of the ACL injury. The medial and lateral meniscus are the cartilage rings which sit on thee inside and outside of the knee. Some meniscus tears can be repaired (fixed), others need to be trimmed back so that the torn edges are smooth (partial meniscectomy). Whether or not the meniscus can be fixed or need to be trimmed depends on the location, the size, and the age of the tear. All attempts are made to try and repair a meniscus that will heal. In some cases, there is also injury to the articular cartilage (the cartilage surface of the knee). The MRI will usually detect this injury, but in some cases it is not seen. This injury will also be addressed at the time of surgery, if necessary.
What are the treatment options for ACL injuries?
The ACL cannot heal on its own, but not all tears of the ACL need to be fixed with surgery. Whether or not the ACL needs to be treated depends on your desired activity level. The ACL is most important with cutting and twisting sports, such as tennis, basketball, soccer, skiing, etc. People with strenuous jobs involving heavy lifting and climbing also usually need their ACL. People who are unwilling or unable to modify their activities and desire an unrestricted lifestyle are encouraged to consider ACL surgery.
People who lead a more sedentary lifestyle may be able to get by with exercise and a brace to stabilize the knee. However, some people may experience instability with simple activities such as going down stairs or stepping off a curb. In these cases, surgery is recommended to restore normal everyday activities and prevent further damage to the knee.
Since the ACL does not heal, the ligament needs to be replaced (reconstructed). The ACL is reconstructed using arthroscopic assisted techniques. The arthroscope is a fiber optic instrument (narrower than a pen) which is put into the knee joint through small incisions. A camera is attached to the arthroscope and the image is viewed on a TV monitor. The arthroscope allows me to fully evaluate the entire knee joint, including the kneecap (patella), the cartilage surfaces, the meniscus, the ligaments (ACL & PCL), and the joint lining. Small instruments ranging from 3-5 millimeters in size are inserted through the incisions so that I can feel the joint structures for any damage, diagnose the injury, and then repair, reconstruct, or remove the damaged tissue.
In ACL reconstruction, a replacement graft (ligament) is positioned in the joint at the site of the former ACL and then fixed to the thigh and lower leg using a metal button, and small plate with post. Although the ACL reconstruction is performed primarily with arthroscopy, a small open incision is needed to place the ligament in the knee. Depending on the type of ligament graft used, and incision may be needed to obtain (harvest) the graft from your knee.
What kind of graft is used for the new ligament?
Choices for the type of replacement graft include autografts (using your own tissue) or allografts (donor tissue from a cadaver). Autograft tissue used for ACL Reconstruction can either be from your patellar tendon (central 1/3 patellar tendon) or the hamstring tendons. The central 1/3 patellar tendon is taken with a small piece of bone from the patella and the tibia. It requires an incision on the front of the knee. It is the graft that has been used the longest, and is the most common graft performed. It has excellent long-term results, and is the graft used for most professional athletes. The disadvantage of a patellar tendon graft is that it can cause more pain for the first several weeks after surgery, and can lead to pain in the front of the knee in a small number of patients.
A hamstring autograft is taken from a small incision towards the inside of the knee. The graft also has excellent results, but has not been used as long as the patellar tendon grafts. Its disadvantage is it can lead to some weakness in the hamstring muscles. It is commonly used in patients who may be predisposed towards pain in the front of the knee.
Allograft tissue is tissue donated from a cadaver. They are also strong grafts with excellent results for ACL reconstruction. Because the tissue is not taken form your body, the surgical time and operative pain is less. This allows generally for an easier rehabilitation. The tissue is rigorously screened for infections, including HIV and Hepatitis. The disadvantage to the allograft tissue is that it has a slightly increased failure rate compared to the autograft tissue.
What are some of the possible complications of surgery?
While complications are not common, all surgery has associated risk. Possible complications include stiffness of the knee after surgery or continued pain. The use of arthroscopic techniques attempts to limit these complications. In addition, there is a risk of continued instability or rupture of the ACL graft. Other complications include an infection, bleeding, nerve damage, blood clots, or problems with the anesthesia.
When should my surgery be performed?
ACL surgery is not an emergency. In fact, it is extremely important that we delay your surgery until some of the inflammation in your knee quiets down. The goal of waiting is to allow you to regain full motion back in your knee prior to surgery. In general, this takes 2 to 3 weeks for most patients, but it can vary. The reason to wait until full motion is achieved is that loss of motion before surgery can make it more likely for the knee to become stiff after surgery.
What kind of anesthesia is used?
ACL reconstruction is usually performed with general anesthesia (going to sleep). If you go home the same day you will be given a femoral nerve block to control post-operative pain.
What do I need to do to prepare for surgery?
Our staff will help to set up the surgery through your insurance company and will instruct you on any paperwork that may be necessary. If you are over the age of 50, or have significant health conditions you may require an EKG and chest x-ray. You may also need to see your internist or family doctor to obtain a Letter of Medical Clearance. The day before the surgery, a member of the hospital or surgery center staff will contact you about what time to arrive for surgery. You may not eat or drink anything after midnight before your surgery.
How long will I be in the hospital?
Most patients are able to go home the same day; rarely others spend the night for a 23-hour stay. This depends on your comfort level with going home and managing the post-operative pain on your own. I will talk with you more extensively about it in the office and in the hospital the day of surgery.
What happens the day of surgery?
The day before surgery you will be told what time to report to the hospital or surgery center. You will be admitted and taken to a pre-operative holding area where you are prepared for surgery. You will be asked several times which extremity I am operating on. Please note that you are asked this question many times on purpose.
After the operation you will be taken to the recovery room to be monitored. Once the effects on anesthesia have worn off and your pain is under good control, you will be given your post-operative instructions and prescription for pain medication and released.
Please be aware that the process of getting checked in, prepared for surgery, undergoing the operation, and recovering from anesthesia takes the majority of the day. I would recommend that you and your family members bring along some reading material to make the process easier for all.
How should I care for my knee after surgery?
Prior to your discharge, you will be given specific instructions on how to care for your knee. In general you can expect the following:
Medication:
You will be given a prescription for pain medication.
Showering:
You may shower, but you should keep the dressing dry. After your dressing is removed you may get your knee wet. You cannot take a bath until the wounds are completely sealed, usually 2-3 weeks after surgery.
Crutches:
You will be instructed how to use crutches before the surgery. You should bring a set of crutches with you to the surgery. Crutches are commonly used for the first 1 to 2 weeks post-op. The therapist will work with you to get you off your crutches when it is safe.
Brace:
You will receive a brace for your knee that you will wear for the first two to four weeks after surgery. The brace is locked in full extension (knee straight) because that is the hardest motion to get back after surgery. When you are not walking you may take the brace off intermittently to work on your exercises.
Diet:
Resume your regular diet as soon as tolerated. It is best to start with clear liquids before advancing to solid food.
Ice:
You should apply ice over the dressing for 20 -30 minutes every hour for several days. Do not use heat for the first 48-72 hours. You may be supplied with a continuous cold therapy unit, use this as directed.
Suture removal:
Your stitches will be removed at your two-week office visit.
Exercise:
You will be instructed on exercises you can begin immediately after the surgery.
Return to work or school:
Your physician will talk with you regarding returning to work or school. Return depends on pain levels and comfort with ambulation with crutches.
What will rehabilitation involve?
The rehabilitation is based on several goals:
- Allowing the tissue to heal
- Regaining motion
- Regaining strength
- Return to sports or work activity
The most important part of the rehabilitation program initially is making sure the knee gets complete extension (totally straight). Following this, the emphasis is to get your knee bending properly. The rehab program is just as important as the surgery in achieving a good result. Typically you will be in therapy 2 times per week for 3-4 months.

When can I return to sports or full duty at work?
In general, you will be allowed to return to sports in four to six months after surgery. You must have good motion, strength, and control of your knee. How quickly you return to sports depends on several factors, including:
- Your own rate of healing
- The damage found at surgery
- If you have any complications
- How well you follow the post-operative instructions
- How hard you work in rehabilitation
In most cases, it will take six months to return to cutting and pivoting sports. When you are able to return to full duty at work depends on your job requirements. I will help to spell those out more clearly at your office visits.
Will I need a brace after surgery for sports?
If I do a good surgery, and you do a good rehabilitation, you do not need a brace after ACL reconstruction. Occasionally, I will have a patient that requests to use a brace of the first year, and that is OK.
Success
Overall, ACL reconstruction is a highly successful operation. The advances in surgical techniques and rehabilitation have led to a 95% success rate for achieving a stable knee following surgery.
To Schedule an appointment with one of our Sports Medicine Specialist please call: (314) 336-2555.
Foot & Ankle
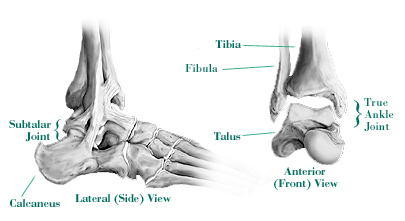

The ankle joint is composed of the tibia (larger leg bone), the fibula (smaller leg bone), and the talus (foot bone). These bones are connected by ligaments which are not visible on routine x-rays. The ankle joint allows up and down (dorsiflexion & plantarflexion) motion of the foot.
The foot is composed on 26 bones connected by ligaments. The talus is the first bone and is part of the ankle joint. Below the talus is the calcaneus (heel bone). The joint between the talus and calcaneus is the subtalar joint. This joint allows the foot to move in and out (inversion & eversion). The foot is divided into 3 sections: the hindfoot (subtalar joint and transverse tarsal joints), the midfoot, and the forefoot (ball of the foot and toes).
Injuries to the ligaments of the foot and ankle are called sprains. Ankle sprains are common sports related injuries occurring with excessive inversion of the hindfoot and ankle. Fractures (or broken bones) occur in the foot and ankle. These are treated with a variety of methods depending on the location and extent of the injury: symptomatic treatment (no treatment other than to control symptoms), surgical shoe, boot, cast, or surgery. Arthritis affects the ankle, hindfoot, midfoot, and forefoot. It is a loss of cartilage in the joint causing friction, inflammation, and pain.